Conditions
Our Services
Diabetic Retinopathy Treatment
- Background Diabetic Retinopathy
- Proliferative Diabetic Retinopathy
- Vitreous Hemorrhage
- Traction Retinal Detachment
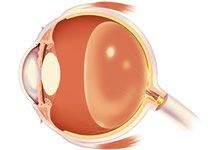
In diabetic retinopathy, the blood vessels of the retina become abnormal and cause the problems that diabetic patients have with their eyesight. Normally, the blood vessels in the retina do not leak. But with diabetes, the retinal blood vessels can develop tiny leaks. These leaks cause fluid or blood to seep into the retina. The retina then becomes wet and cannot work properly. The form of diabetic retinopathy caused by leakage of the retinal blood vessels is called background diabetic retinopathy
(BDR)/non-proliferative diabetic retinopathy (NPDR).
Another problem with the retinal blood vessels in diabetes is that they can close. The retinal tissue, which depends on those vessels for nutrition, will no longer work properly. The areas of the retina in which the blood vessels have closed then foster the growth of abnormal new blood vessels that can be very bad for the eye, as they can cause bleeding and scar tissue that may result in a severe or total loss of vision. The form of diabetic retinopathy caused by closure of the blood vessels from which abnormal new blood vessels grow is called proliferative diabetic retinopathy
(PDR). This more advanced stage can lead to severe vision loss through the development of vitreous hemorrhage
and/or traction retinal detachment.
If you would like more information about Diabetic Retinopathy Treatment, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
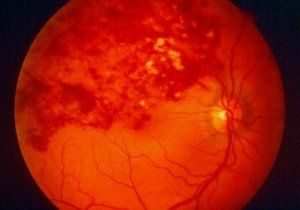
Background Diabetic Retinopathy/Non-Proliferative Retinopathy (NPDR)
In diabetes, the retinal blood vessels can develop tiny leaks. Blood and fluid seep from the retinal blood vessels, and fatty material, called exudate, may deposit in the retina. This may be associated with swelling of the retina, and it is called nonproliferative diabetic retinopathy (NPDR). When the swelling occurs in the central part of the retina (the macula), it is called macular edema and vision may be reduced or blurred. Leakage elsewhere in the retina will usually have no effect on vision.

A patient with a wet, swollen macula, with or with exudate in the macula, will experience some loss of vision, including blurring, distortion, or darkening. If one eye is affected, the other eye is frequently affected also, though the problem may not be equally severe in both eyes. If the diabetic retinopathy has affected each macula severely, central vision may be lost from each eye. But even if the ability to see detail has been lost from both eyes, the person with severe NPDR will usually be able to get along fairly well by learning to use the area just outside of the macula to see some detail. This ability to look slightly off center usually improves with time, though the eyesight will never be as good as it was before the macula was damaged by the leakage of blood vessels. So patients who have NPDR will usually be able to see well enough to take care of themselves and continue those activities that do not require detailed vision.
Early Diagnosis of Nonproliferative Diabetic Retinopathy
Amsler Grid Self Test
It is important that patients be aware of what they are seeing with each eye. If a patient can detect a problem with vision very early, the chance of saving eyesight with laser surgery is much greater. Once the macula has been damaged, laser surgery is generally not as helpful. For this reason, everyone should test the vision in each eye, separately, each day.
One way to test vision in order to detect even small changes when they first appear is to use the Amsler grid. Follow these instructions:

- Wear your reading glasses and hold the Amsler grid at a normal reading distance.
- Cover one eye.
- Look at the center dot and keep looking at it at all times.
- While looking directly at the center, be sure that all the lines are straight and all the small squares are the same size.
- If you should notice any changes on the grid such as distortion, blur, discoloration, or other abnormality, and it stays that way for a few days, call and see your eye doctor right away.
- Be sure to test the other eye in the same manner.
Laser Surgery for Diabetic Retinopathy
The laser is used to stop abnormal retinal blood vessels from leaking fluid into the retina. Vision does not usually improve with a laser, but laser treatments can frequently stop further loss of vision. When the swelling of the retina or amount of exudate in the macula has reached a critical stage, laser treatments should be performed so that vision does not deteriorate further. Your own doctor can help you evaluate your chances with laser surgery and discuss the options with you.
There are two types of laser surgery for NPDR: Focal (or specific) surgery
and Grid surgery. With focal laser surgery, the specific leaking spots in the retina are found by a fluorescein angiogram, which is then used as a guide for the laser in an attempt to stop the leakage. In some patients, all of the leaking spots may be properly treated. In others, all of the leaking spots may be properly treated, but they may continue to leak, or new ones may develop. In such cases, further leakage causes more swelling and worsening of vision. Additional laser surgery frequently needs to be done in order to stop new leakage, but again, the vision is not likely to improve. In other situations, further laser surgery is not helpful and should not be done.
In some cases of NPDR, blood vessels appear to be leaking everywhere in the macula and not just in a few specific areas. In such cases, a scatter of laser energy in a grid pattern is placed across the entire swollen macular area. Grid laser surgery has a fair chance of drying the macula and holding vision stable. Grid surgery, however, infrequently improves vision. Again your doctor will help you evaluate whether specific (focal) or grid surgery, or a combination of the two, is best.
Grid Laser of Diffuse Diabetic Macular Edema
After the laser surgery, the patient will often see the many small spots caused by laser burns. With time, the spots tend to shrink and fade, and the patient will be less bothered by them, though they will always be there.
Even when laser surgery has successfully sealed the leaking vessels, new areas of leakage frequently appear later, causing more swelling and more loss of vision. The patient who is treated with laser should continue to check the vision in each eye daily and tell the doctor immediately if there are new changes, such as a return of distortion or blurriness. Vision does not usually improve with laser surgery, but if NPDR is discovered early enough, laser surgery may stop further loss.
Anti VEGF therapy for Diabetic Macular Edema
VEGF (Vascular endotheilial growth factor) is the chemical in the retina that causes blood vessels to leak resulting in diabetic macular edema. Recent studies have shown that anti-VEGF injections of either Avastin or Lucentis into the eye are very effective in treating diabetic macular edema. Thus, either Anti-VEGF alone or in combination with laser treatment appears to be the better treatment for macular edema in certain patients. Studies however are ongoing.
If you would like more information about Background Diabetic Retinopathy/Non-Proliferative Retinopathy (NPDR), or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
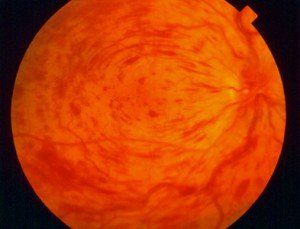
Proliferative Diabetic Retinopathy
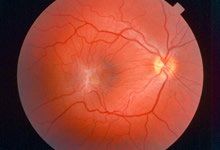
In PDR, retinal blood vessels close off, and large areas of retina lose their source of nutrition. When this happens, peripheral or side vision is usually reduced, and the patient’s ability to see at night and to adjust from light to dark is often diminished.
As a result of this loss of nourishing blood flow, the retina responds by developing new blood vessels that are abnormal and are called neovascularization. The development of neovascularization is the retina’s method of coping with the closing of its own blood vessels and the loss of nourishment. Many people with diabetes have some closing of retinal blood vessels without ever developing neovascularization. But the problem is that when neovascularization develops, it is never always a problem. It is, in fact, dangerous to the eye. Neovascularization does not nourish the retina properly, and it may cause other problems. One problem is bleeding into the vitreous cavity (called vitreous hemorrhage). A second problem that occurs when neovascularization develops is the growth of scar tissue on the retina; the scar tissue can pull the retina off the back wall of the eye (called a traction retinal detachment). Either of these serious problems, vitreous hemorrhage or traction retinal detachment, can lead to severe loss of vision or even total blindness.
A third problem that can occur is when neovascularization grows on the iris, the colored part of the eye, rather than just on the retina. When neovascularization grows on the iris (called rubeosis), it may close off normal flow of fluid out of the eye and cause the pressure in the eye to rise to dangerously high levels. The high pressure (called neovascular glaucoma) can cause permanent changes, resulting in visual loss, pain, or even loss of the eye.
It is very important to understand that the closing of retinal blood vessels and the development and growth of neovascularization may occur without any noticeable change of vision. So, it may be impossible for the person with diabetes and early PDR to know that such changes are occurring. For this reason, it is essential that every person with diabetes be examined regularly by a specialist who is familiar with diagnosing diabetic retinopathy. Such examinations should occur regularly–probably every six to twelve months, or more or less frequently–for the lifetime of the person with diabetes. The earlier neovascularization is discovered, the better the chance that laser surgery
will save vision. The later neovascularization is discovered, the greater the chance for blindness.
All people with diabetes should be examined regularly to be sure that neovascularization is not developing. When neovascularization does develop, if the amount is not severe, laser surgery is not necessary as long as the patient is examined regularly.
If the amount of neovascularization is great, laser surgery can often prevent loss of vision. The type of laser surgery that is done when there is a lot of neovascularization is called pan retinal laser photocoagulation. This type of laser surgery is usually done in two or more separate sessions. The idea is to use the laser to destroy all of the dead areas of retina where the blood vessels have been closed. When these areas are treated with the laser, the retina stops manufacturing new blood vessels, and those that are already present tend to decrease or disappear.
Pan Retinal Photocoagulation
There are side effects of pan retinal laser photocoagulation and, for this reason, this surgery is not done when only a small amount of neovascularization is present. It is important to remember, however, that when the amount is great enough to warrant laser surgery, the longer the eye remains untreated the more likely vision will be lost and blindness will occur. The earlier severe neovascularization is discovered and the eye is treated with laser, the more likely blindness can be prevented. If you have developed neovascularization, your doctor will advise you about when pan retinal laser photocoagulation should be done.
Pan retinal laser photocoagulation does not improve vision, however, it is the best possible means of holding vision stable to prevent further loss. After laser surgery, patients may still have reduced vision or may continue to lose more vision. But if pan retinal laser photocoagulation is indicated, the chances are that it will prevent severe loss of vision.
Pan retinal laser photocoagulation is placed on the side (periphery) of the retina, not on the center, and side (peripheral) vision will definitely be diminished to some extent. These side areas are sacrificed in order to save as much of the central vision as possible and to save the eye itself. Night vision will also be diminished. After laser, blurred vision is very common. Usually, this blur goes away, but in a small number of patients, some blur will continue forever.
Because diabetic retinopathy can occur at any time, the patient who is treated with laser for either NPDR or PDR should have regular retinal examinations by an eye specialist.
If you would like more information about Background Proliferative Diabetic Retinopathy, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Vitreous Hemorrhage
Because vitreous hemorrhage is not necessarily associated with any specific activity (although it can be associated with strenuous physical activity), people with diabetes are encouraged to have regular eye exams, and your doctor will help advise you. When a person does notice the sudden appearance of floaters, spider webs, spots in front of the eye, or blurred vision, they should immediately call their eye doctor. Vitreous hemorrhage in a diabetic is most often associated with the stage known as proliferative diabetic retinopathy (PDR).

Treatment
It is often helpful for someone with diabetes who develops a vitreous hemorrhage to remain in a sitting position so that gravity can help settle the blood to the lower parts of vitreous cavity. Once the blood settles, pan-retinal laser photocoagulation can be performed. Laser surgery
cannot make the blood disappear, but it can cause the neovascularization (new abnormal blood vessels) that bled, to shrink and thereby prevent more bleeding into the vitreous. The vitreous hemorrhage that is present usually disappears with time but can take many months to clear.
If there is so much vitreous hemorrhage that laser surgery is not possible, or if the blood does not disappear on its own in a reasonable period of time, it can be removed with an operation called a vitrectomy.
Vitrectomy surgery is done in the hospital, under general or local anesthesia. The blood-filled vitreous gel is removed. It is replaced during the operation with clear fluid that is compatible with the eye. Endolaser photocoagulation is often performed simultaneously to help stabilize the proliferative diabetic retina. Over time, the fluid is absorbed by the eye and is replaced by the eye’s own fluid, although the eye does not replace the gel itself. The lack of vitreous gel does not affect the function of the eye. If the blood in the vitreous does not go away on its own, your doctor will advise you as to how long you should wait before vitrectomy surgery is considered.
If you would like more information about Vitreous Hemorrhage, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Retinal Detachment
Retinal Detachment Repair
Rhegmatogenous Retinal Detachment
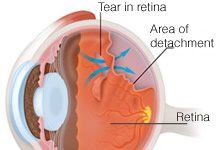
The most common variety of retinal detachment results from a hole or tear, usually but not always in the periphery, which allows fluid to migrate under the edges of the break, and detach the retina. A limited detachment may be treated by laser surgery
if the macula is not theatened. More extensive fluid build-up will require gas bubble, or Scleral Buckling, and/or vitrectomy
surgery with fluid-air exchange. More complicated cases especially re-operations for the same condition may require silicone oil.
Tractional Retinal Detachment
This type of detachment usually involves other retinal disorders, i.e., diabetes, vascular occlusion, inflammation, and prior trauma, including prior surgery. Successful treatment involves removing fibrovascular scar tissue, in the case of vascular-related diseases, utilizing micro-vitreo-retinal surgery to desegment and peel the membrane to eliminate the tractional forces. In the case of re-operations and/or trauma-related detachments, a special condition known as Proliferative vitreoretinopathy
(PVR), which is mostly very adherent fibrous scar tissue causing mostly tangential traction, requires meticulous dissection and/or cutting of the retina in order to relieve the pulling forces. This is usually followed by long-acting gas or silicone oil.
If you would like more information about Retinal Detachment Repair, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Traction Retinal Detachment
In proliferative diabetic retinopathy
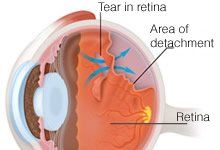
(PDR), the neovascularization may cause scar tissue to develop. The neovascularization and the scar tissue grow along the surface of the retina and attach firmly to the back surface of the vitreous gel. The vitreous gel pulls on the blood vessels and scar tissue and lifts them up. Because the neovascularization and scar tissue are attached to the retina, the retina is also lifted up. When the retina separates from the back surface of the eye, it is called a retinal detachment. Because the retina is pulled off, it is called a traction retinal detachment. The scar tissue can also tear the retina and cause a retinal detachment. Vitreous hemorrhage may also accompany the tractional process.

When a retinal detachment occurs, the patient may notice a shadow or very large dark area in the vision. When the retinal detachment extends to the macula, the dark shadow will be straight ahead and vision may be poor. The neovascularization and scar tissue also can cause visual loss because of surface wrinkling of the retina.
The only way the patient can regain any vision is for the retina to be reattached and the neovascularization and scar tissue to be removed from the surface of the retina. This is accomplished by vitrectomy
surgery. The surgeon removes the vitreous gel from the eye so that it stops pulling on the retina; and the traction is released. The surgeon may remove the scar tissue from the surface of the retina so that there is no wrinkling of the retina. The detached and wrinkled retina should flatten and smooth out. The surgeon may also perform endolaser photocoagulation to prevent further development of neovascularization and rubeosis irides.
The surgeon may also use the endolaser to seal any tears or breaks in the retina. If there are tears in the retina, the surgeon may place a large gas bubble in the eye to press the retina completely against the back wall of the eye while the laser surgery takes hold. In time, the gas bubble will disappear and be replaced by the eye’s own fluid.
If you would like more information about Traction Retinal Detachment, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Cryotherapy and Scleral Buckling
If the retina has become detached and the detachment is too large for laser treatment or cryotherapy alone, surgery is necessary to “reattach” the retina. Without some type of retinal reattachment surgery, vision will almost always be completely lost. If pneumatic retinopexy cannot be performed, a pars plana vitrectomy
with or without a scleral buckle is usually the procedure used to repair the retinal detached retina.
The Procedure
Scleral Buckling
is generally performed in the operating room under local anesthesia but, in some cases, may be performed under general anesthesia. The surgeon first treats the retinal tear with cryotherapy, first looking into the eye using a cryoprobe placed on the outside part of the eye (the sclera). The surgeon then places the cryoprobe in the correct position and the retinal tear is treated. A piece of silicone plastic or sponge is then sewn onto the outside wall of the eye (sclera) over the site of the retinal tear. This pushes the sclera in toward the retinal tear and holds the retina against the sclera until scarring from the cryotherapy seals the tear. This surgery is called scleral buckling because the sclera is buckled (pushed) in by the silicone. The silicone buckle is left on the eye permanently.
The silicone may also be placed all around the outside circumference of the eye. This is called an encircling scleral buckle or band. The purpose of the encircling scleral buckle is to lessen the pulling of the vitreous on the retina. During the surgery, the surgeon may drain the fluid from beneath the retina by making a tiny slit in the sclera, and then making a small puncture into the space under the retina. The fluid under the retina then drains out through the slit in the sclera.
Encircling Scleral Buckle
Occasionally, the surgeon may place a gas bubble into the vitreous cavity. When the surgery is over, the patient is positioned so that the gas bubble
rises and pushes the retinal tear against the scleral buckle to help keep the tear closed.
In most cases, there is a better than 80% chance of successfully reattaching the retina with one operation. But successful reattachment does not necessarily mean restored vision. The return of good vision after surgery depends on whether, and for how long, the macula was detached prior to surgery. If the macula was detached, vision rarely returns to normal. Still, if the retina is successfully reattached, vision usually improves. The best vision may not occur for many months after surgery.
Postoperative Period
Following surgery, the eye will be red and slightly sore for a month or two. Patients often feel a scratchy sensation produced by the stitches used to close the lining around the eye. Severe pain is uncommon; if it occurs, the surgeon should be told immediately. The eye will water for several weeks, and the patient may find it more comfortable to wear a patch on the operated eye. Usually, several medications given as eye drops must be taken after the surgery. These should be continued until the surgeon asks the patient to stop. These drops are used to prevent infection and to help make the eye feel more comfortable. In most cases, the patient may leave the hospital the day of surgery.
Following the surgery, vision will be blurry; it may take many weeks for the vision to improve. During this period the main concern is that the retina remains attached. Many surgeons ask their patients to restrict their physical activity for several weeks.
Complication of Scleral Buckling
Even though the surgery for retinal detachment is generally successful, certain complications can occur. Any one of these complications can result in failure of the operations, loss of some or all vision, and, in rare situations, even loss of the eye.
Retinal detachment surgery done by scleral buckling can affect the eye muscles that move the eye and keep the eye straight. This can result in double vision, which on rare occasions is permanent. Retinal detachment surgery can also cause bleeding under the retina, cataract formation, glaucoma, retinal redetachment, proliferative retinopathy, vitreous hemorrhage, drooping of the upper lid, and infection. Although any one of these can result in the need for some surgery, or in the total loss of vision, these complications are very infrequent. Retinal redetachment is the most commonly occurring problem. If this occurs, your surgeon will discuss the chance that a reoperation will successfully reattach the retina.
If you would like more information about Cryotherapy and Scleral Buckling, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Pneumatic Retinopexy (Gas Bubble Injection)
Cryotherapy or laser treatment can be performed to seal the retinal tear. The surgeon injects a gas bubble inside the vitreous cavity of the eye using a needle. The patient is instructed to keep his head in a specific position so that the gas bubble pushes the detached retina against the back wall of the eye to seal the retinal tear. The patient is then asked to remain in this position for various periods of time until the retinal tear is sealed against the back wall of the eye. The surgeon will tell you how long special positioning is necessary.
The gas bubble in the vitreous cavity of the eye expands for several days and will take six to eight weeks to disappear. During this time, airplane travel or travel to a high altitude must be avoided because high altitudes can result in an expansion of gas and an increase in pressure that can damage the eye. Your surgeon will tell you when it is safe to travel. It is also important for a patient with a gas bubble not to lie face up, as the air bubble may come to rest against the lens of the eye and cause a cataract or high pressure in the eye.
Outcome
The chance of successfully reattaching the retina with pneumatic retinopexy is less than with the scleral buckling surgery, but the final visual outcome is better if the pneumatic retinopexy is successful. Also, pneumatic retinopexy cannot be used, or is not effective, for every retinal detachment. The surgeon will discuss with you whether pneumatic retinopexy is feasible and the chances for successfully reattaching your retina. With pneumatic retinopexy, hospitalization, general anesthesia, and the cutting done for the scleral buckling surgery are all avoided. Complications of pneumatic retinopexy include cataract formation, glaucoma, gas getting under the retina, excessive scar tissue formation, and infection. Any one of these complications can lead to a total loss of vision, but each is rare. The most common complication is recurrence of the retinal detachment. The recurrence rate is about 25%. If the retina becomes detached again, scleral buckling surgery or vitrectomy
can usually be performed to reattach it.
If you would like more information about Pneumatic Retinopexy (Gas Bubble Injection), or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Proliferative Vitreoretinopathy (PVR)
Proliferative vitreoretinopathy (PVR) involves the growth of scar tissue around the vitreous and retina of the eye. It is typically a complication of retinal detachment, a disorder that occurs when the retina is pulled away from the underlying tissue to which it is normally attached. The scar tissue cells of PVR form in the area of the injury and may continue to expand even after a surgeon has corrected the detachment. This results in a tugging on the retina that can cause another detachment in either the same area as the initial problem or elsewhere along the retina. The patient may have symptoms such as visual disturbances and loss of vision.

It is essential to treat PVR as soon as possible to prevent permanent vision loss. This condition is often repaired with a procedure known as a pars plana vitrectomy. A pars plana vitrectomy
removes the natural vitreous by suctioning it out with tiny instruments inserted into the eye. The vitreous is then replaced with fluid. The retina may be treated with a laser to cut or remove the scar tissue, flatten detached areas of the retina and repair any holes or tears that have formed. While results vary depending on the severity of the condition treated, most patients experience an improved visual acuity after the procedure.
If you would like more information about Proliferative Vitreoretinopathy (PVR), or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Macular Hole & Pucker Treatments
Macular Holes Treatment
A macular hole is a relatively uncommon cause for loss of central vision. The first symptoms of macular hole may be slight distortion of vision, which soon progresses to a blind spot in the central vision. The symptoms of macular hole resemble those of macular degeneration initially. Macular degeneration is a totally different problem but occurs in the same place as macular hole. OCT imaging can greatly aid in the diagnosis of this condition.

Macular holes are treated by an outpatient surgical procedure called vitrectomy, membrane peeling and gas fluid exchange. The central gel is removed. The epiretinal membrane is removed from the surface of the macula. The eye is then filled with a special gas bubble. Postoperatively, the patient must be positioned so that the face is down. In this position, the force of the bubble seals the hole. This position must be maintained for 3 days, although that may vary depending on the individual. There are several companies that provide equipment to support patients in maintaining the face-down position.
After surgery, the bubble will fill the eye, causing blurred vision when looking straight ahead. However, if the patient looks down and brings an object within a few inches of the eye, the patient will be able to see it clearly. Over time, the bubble dissolves. It may appear as a line in the vision and then gradually get smaller until one day it totally disappears. The time to dissolve depends on the type of gas used. While the bubble is present, the patient is restricted from flying in an airplane and from going to high elevations because this may cause the bubble to expand in the eye, resulting in severe glaucoma and loss of vision.The surgery for macular hole has a success rate of over 90%. The visual outcome depends a lot on how soon the surgery is done and how well the patient complies with face down positioning. The better the vision is before the surgery, the better the chance for a good outcome.
Epiretinal Membrane (Macular Pucker) Treatment
An epiretinal membrane, also known as a macular pucker, is a thin layer of scar tissue that forms over the macula, the area of the retina that gives us clear central vision. An epiretinal membrane often develops with age, as the vitreous gel that makes up most of the eye’s volume thins and pulls away from the retina. The damage caused to the retina leads to the formation of scar tissue on the retina. When the scar tissue contracts, the retina wrinkles, or puckers, causing blurry or distorted central vision.
Patients with an epiretinal membrane may experience difficulty seeing fine details and reading small print, and may also see straight lines appearing as wavy. There may also be a gray area or blind spot in the center of your vision. Although the cause of these conditions is similar, an epiretinal membrane is different from a macular hole. A macular hole is usually a much more serious condition that can progressively worsen.
Most cases of epiretinal membranes do not progress and do not require treatment. The symptoms of distortion and blurriness are usually mild, and patients are able to adjust to the vision changes without much impact on their daily lives. Noninvasive treatments such as eye drops or medications will not improve vision that is distorted from an epiretinal membrane. If vision distortion is severe enough, a vitrectomy
may be performed to repair this condition.
If you would like more information about Macular Hole & Pucker Treatments, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Peripheral & Giant Retinal Tears
Peripheral Tears
As the vitreous pulls away from the retina during a posterior vitreous detachment, the retina may at times tear. Retinal detachment
occurs if fluid from within the vitreous passes through the tear and collects under the retina, causing the retina the separate from the underlying tissue (retinal pigment epithelium). The retinal tear may be associated with the symptoms of a posterior vitreous detachment (flashing lights and floaters). However as most retinal tears occur in the more peripheral parts of the retina, a retinal tear will usually not cause loss of vision unless there is progression to retinal detachment. The detached retina is not capable of normal sight and as the retinal detachment enlarges and approaches the central part of the retina there will be an enlarging area of vision loss. This is sometimes described as a shadow or veil covering the vision. Sometimes retinal tears occur without associated floaters or flashing lights. In these cases, the first symptoms to occur may be the loss of vision due to retinal detachment.
Not all retinal tears will lead to retinal detachment. At times, a retinal hole or tear may be found during a routine eye exam without there having been any associated symptoms. In this situation the risk of progression to retinal detachment may be low and treatment of the retinal tear in this situation may not always be needed. However, retinal tears associated with symptoms suggesting that there has been a recent posterior vitreous detachment are usually felt to be of high risk of progression to retinal detachment and should, under most circumstances be treated in order to minimize the risk of progression to retinal detachment. Retinal tears, if detected early, can usually be treated by lasers.
Giant Retinal Tears
Retinal tears that are very large, extending across at least one quarter of the retina, are called giant retinal tears. This is a serious condition that can result in the retina folding over upon itself and causing vision loss.
Several types of treatments may be employed to repair a giant retinal tear. A vitrectomy is performed to remove the clear, gel-like substance known as the vitreous to which the retina is normally attached. Perfluorocarbon liquid can be very successful in unfolding the retina and restoring it to its correct position. This will help reattach the retina and seal it in place, followed by wither long-acting gas or silicone oil. In most cases, lasers
are used to repair the tear and hold the retina in position. A scleral buckle can benefit some patients as well. This is a thin strip of silicone that is secured around the eyeball to relieve the pull on the retina and narrow the space between the two layers of the retina that have torn apart.
Many surgeries to repair a giant retinal tear are successful. Complications such as PVR, which is the development of scar tissue on the retina, are not uncommon and may necessitate another procedure at some point. Vision will take time to improve after a giant retinal tear repair and it may not return to previous levels of acuity.
If you would like more information about Peripheral & Giant Retinal Tears, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Laser Retina Surgery
Laser retina surgery can be used to treat a wide range of retinal conditions through minimally invasive techniques that produce long-lasting results. These diseases can often lead to serious complications such as hemorrhaging and blindness. Lasers have been used to treat eye diseases for more than 30 years and produce effective results with no damage to surrounding tissue and no need for needles.
Laser surgery can be used to treat diabetic retinopathy, retinal vein occlusions, age-related macular degeneration, retinal detachments
and more. Depending on the patient's condition, the laser may be used to seal leaking blood vessels, repair tears, remove newly formed blood vessels or destroy tumors. These procedures are performed in the doctor's office and require only anesthetic eye drops to numb the area prior to treatment. Laser treatment usually takes less than 30 minutes to perform, and patients can go home immediately following surgery. Most patients return to work and other normal activities the next day.
Several laser treatments may be needed in order to achieve optimal results and to help manage chronic retinal conditions. Results may take a few weeks or months to become noticeable, so it is important to see your doctor for follow-up appointments in order to ensure that you receive the best possible results.
Focal Photocoagulation
Retinal laser photocoagulation is a minimally invasive procedure used to seal or destroy leaking blood vessels in the retina that lead to serious retinal conditions such as diabetic retinopathy and macular edema. This procedure can also seal retinal tears and destroy abnormal tissue found in the back of the eye.
Focal laser coagulation may be recommended for patients with clinically significant macular edema (CSME) - swelling of the central retina, called the macula. The laser coagulates, or dries up, the fluid that is causing the swelling. During focal photocoagulation, laser burns are made on the retina to target leaking blood vessels. While it cannot restore vision that has already been lost, it can reduce the risk of vision loss.
This procedure is performed with a local or topical anesthetic on an outpatient basis. Patients will need someone to drive them home after the procedure, since the pupils will be dilated for several hours. Your vision may also be blurry and you may experience mild pain for a day or two after the procedure. You can resume normal activities immediately.
Laser photocoagulation carries certain risks, since it involves burning and destroying part of the retina. Patients may experience a mild loss of central vision, reduced night vision and a decreased ability to focus. However, the potential vision loss caused by this procedure is far less than the severe vision loss that can occur as a result of retinal conditions like diabetic retinopathy.
Pan Retinal Photocoagulation
Pan retinal photocoagulation is a more extensive variation on focal photocoagulation. It is used to treat the entire area to slow the growth of new abnormal vessels. This form of treatment is reserved for more serious cases of retinopathy.
During pan retinal photocoagulation, a laser is applied to all portions of the retina with blood vessel damage and tissue that has not received enough oxygen. The blood vessels will shrink, and new ones are not created. This can lower your risk of further vision loss due to a retinal detachment or vitreous hemorrhage.
Multi-Pulse Technology
A newer form of pan retinal photocoagulation, multi-pulse technology allows the doctor to control the timing and intensity of the laser pulses in order to curtail treatment time and maximize precision. These short pulses are applied to the abnormal blood vessels mere milliseconds apart, providing a greater level of safety to the patient because it can be more precisely targeted and reduce the likelihood of damage to the nearby epithelium.
Thermal laser/Photodynamic Therapy
Thermal laser is used to treat extra-macular choroidal noevascular membranes which can complicate age-realated macular degeneration, degenerative myopia, and other choroidal disorders, in which leaks form beneath the retina. These leaks occur in a structure in the eye called the choroidal neovascular membrane, or CNVM. Photodynamic therapy is used to treat a complication of wet macular degeneration that may located closer to the center of the macula, especially when anti-VEGF treatment is contra-indicated or fails. During photodynamic therapy, dye is injected into the CNVM and a narrow-wavelength laser beam is focused on it for about 90 seconds. The dye absorbs the energy and slows or stops leakage by creating blood clots and stopping abnormal blood vessels from growing. Following treatment, patients should avoid direct exposure to sunlight for several days. Patients most likely to benefit from treatment will have newly onset macular degeneration and no scarring. Vision stabilization is maximized with a series of treatments over one to two years.
If you would like more information about Laser Retina Surgery, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Intravitreal Injection
Anti-VEGF pharmaceuticals
Anti-vascular endothelial growth factor (VEGF) is a molecule specifically designed to block the damaging effects of VEGF, which is elaborated, typically, by neovascular tissue. The major benefit in selecting an anti-VEGF compound rests in the critical location of the neovascular tissue, and the need to avoid tissue-destroying approaches at or near the center of the macula. The variety of agents available for intra-vitreal injection include Avastin, Lucentis, and Eyelea. The protocol depends on the agent selected, the nature of the problem being treated, and the individual. In over 92% of individuals treated, visual acuity may be stabilized and/or improved.
Steroids
Intravitreal steroid injections of triamcinolone acetate or implantation of sustained-delivery devices may reduce the vascular activity of the neovascular tissue alone or in conjunction with an anti-VEGF agent and/or laser treatment (in susceptible lesions).
If you would like more information about Intravitreal Injection, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
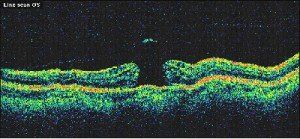
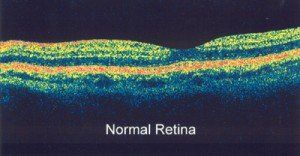
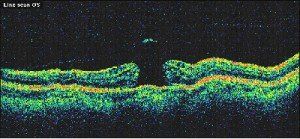
Optical Coherence Tomography (OCT)
Optical coherence tomography, also known as OCT, is an imaging system that uses light waves to produce a high-resolution view of the cross-section of the retina and other structures in the interior of the eye.
Conditions Detected With an OCT
The images can help with the detection and treatment of serious eye conditions such as:
- Macular hole
- Macular swelling
- Optic nerve damage
- Age-related macular degeneration
- Macular pucker
- Diabetic eye disease
OCT uses technology that is similar to that of a CT scan of internal organs. With the scattering of light it can rapidly scan the eye to create an accurate cross-section. Each layer of the retina can be evaluated and measured and compared to normal, healthy images of the retina.
The OCT exam takes about 10 to 20 minutes to perform in your doctor's office, and usually requires dilation of the pupils for the best results.
If you would like more information about Optical Coherence Tomography (OCT), or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Macular Degeneration
If you would like more information about Macular Degeneration, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
What is Macular Degeneration?
Macular degeneration is most often related to aging. There are some unusual types of macular degeneration that start very early in life, however, most patients with macular degeneration begin to notice problems with eyesight sometimes after age 50. Macular degeneration may be hereditary and therefore may run in families. Macular degeneration usually starts with the appearance of spots called drusen on the retina. Drusen are like age spots and do not usually change vision very much themselves. Most patients with drusen never have a serious loss of vision and only a few develop severe macular degeneration with loss of vision.

When macular degeneration does lead to loss of vision, that loss usually starts in just one eye and only later may affect the other eye. In some, it never affects the vision of the second eye. When a person loses vision from macular degeneration in one eye, the loss of vision may not even be noticed because the healthy eye can still see detail.
In general, it is important to discover any change in eyesight as early as possible because the chance that treatment
will help is greatest in the early stages of any eye problem. That is why you should test the eyesight in each eye, each day, especially if your doctor has told you that you have drusen.
If macular degeneration has affected the vision of only one macula, you will still be able to see detail (to read, to drive, to thread a needle) with the other, healthy macula. It is only when macular degeneration severely affects both eyes that it will become difficult, or perhaps impossible to do the kind of work that requires detail vision.
A person with severe macular degeneration, who has lost the ability to see detail with each eye, rarely loses peripheral vision and will still be able to get along fairly well. It is very rare for someone with macular degeneration to lose both macular (detail) and peripheral (side) vision. Macular degeneration only very rarely causes total blindness. Almost all people with severe macular degeneration in each eye can see well enough to take care of themselves and continue those activities that do not require detail vision.
People with macular degeneration in each eye usually learn to make use of the areas just outside the macula to see detail better. This ability to look slightly off center usually improves with time, although eyesight will never be as good as it was before the macula was damaged. Once the macula has been severely damaged, treatment is usually no longer possible. For this reason everyone should test the vision in each eye, separately, each day.
One very good way to test the central vision in order to detect even the smallest changes when they first appear is to use the Amsler grid (see below). If you note any changes you should see your eye doctor promptly.
Amsler Grid Test
Instructions on using the Amsler grid:
- Cover one eye.
- Look at the center dot and keep your eye focused on it at all times.
- While looking directly at the center, and only the center, be sure that all the lines are straight and all the small squares are the same size.
- Wear your reading glasses.
- If you should notice any area on the grid that becomes distorted, blurred, discolored, or otherwise abnormal, please call right away.
- Do this test for each eye separately.
- In the earliest stages of macular degeneration, it may be a little harder to see. Vision may be blurred for distance or for reading, or both.

A very frequent and important symptom is distortion. Straight lines will not look straight. A telephone pole or a door frame may seem a little bent, crooked, or irregular, as though seen through heat waves on a highway. An area of the Amsler grid will appear distorted and the small boxes in that area will vary in shape and size. Also, you may see a dark gray spot similar to the aftereffect caused by a flashbulb. There may be other changes in vision: you may notice that the size of an object appears different for each eye or that colors don’t look the same for each eye. These changes in eyesight are important symptoms and anyone who has these symptoms should make sure that he or she sees the eye doctor promptly. Do not assume you simply need a new pair of glasses and wait for an appointment in the future.
In the earliest stages of macular degeneration, it may be a little harder to see. Vision may be blurred for distance or for reading, or both.
If you would like more information about What is Macular Degeneration?, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Two Forms of Macular Degeneration
There are two main forms of macular degeneration: a dry form and a wet form. There is another form, which is uncommon, called pigment epithelial detachment (PED) that will be discussed later. In order to determine if you have macular degeneration and what form, the doctor will measure your vision and examine your eyes. By looking at the retina, the doctor will be able to tell if there is an abnormality. If drusen are found, you will want to schedule regular check-ups to make sure that no further damage is occurring. It may be necessary that photographs of each macula be taken to use for comparison with future examinations.
Dry or Atrophic Macular Degeneration
Drusen are considered to be a dry form of macular degeneration. When drusen are present for a long time, the macula may thin and stop working. This is referred to as atrophy or atrophic macular degeneration and it often causes a slow and progressive loss of vision.
Although there is no medical or surgical treatment for this form of macular degeneration, eyesight may be helped somewhat with the use of special low vision lenses: Magnifying lenses for close-up and telescopic lenses for distance. With counseling, people can learn to use some of their peripheral vision to help them see more clearly, and to cope more effectively with the practical tasks of every day life. Because the dry form of macular degeneration with drusen or atrophy can change into the wet form, it is important for anyone with the dry form to monitor vision (with the Amsler grid, for example) and report any new changes to their eye doctor.

Although the dry form of macular degeneration with atrophy can cause a large loss of detail vision, the damage done by atrophy is generally not as great as the damage that can be caused by the wet form. The dry form occurs in approximately 85 to 90% of people with macular degeneration. The wet form, which can be even more severe, occurs in only about 10% of people with macular degeneration.
Wet Macular Degeneration
Sub retinal Choroidal Neovascularization–CRNV
In the wet form of macular degeneration, abnormal blood vessels grow under the retina and lift the retina up, very much like the roots of a tree growing under a sidewalk, these abnormal blood vessels are called sub retinal choroidal neovascularization, or CRNV. The abnormal blood vessels located under the retina may leak fluid, bleed, and lift up the retina. When this happens, vision is reduced.
The longer the abnormal blood vessels continue to leak, bleed, and grow, the more detail vision will be lost. An eye with the wet form of macular degeneration will usually lose its ability to see detail. In some cases, laser treatment done promptly may stop or minimize loss of vision but laser treatment does not guarantee that vision won’t be lost. In addition, if the abnormal blood vessels occur in one eye, there is about a one in ten chance per year that they will occur in the other eye.
The earlier that abnormal blood vessels are discovered, the more likely that some or much of the central (detail) vision can be saved. The later abnormal vessels are discovered, the less likely laser treatment can be done. In other words, pay close attention to your eyesight and see your eye doctor promptly if there is any type of change in your vision. fluorescein angiography
and OCT
are used to diagnose and characterize this condition.
Pigment Epithelial Detachment (PED)
There is a third form of macular degeneration that is called pigment epithelial detachment (PED). In this form of macular degeneration a blister (PED) can form in the macula, with or without hemorrhage, causing blurring or distortion of vision. Diagnosis is greatly facilitated using Fluorescein angiography
and OCT. Intra-vitreal anti-VEGF injections
are usually indicated. Laser treatment is not usually recommended unless abnormal blood vessels are also present, and located away from the fovea. If you have a PED, you will want to have your eyes examined regularly to see that the condition does not worsen.

If you would like more information about Two Forms of Macular Degeneration, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Fluorescein Angiography
If your doctor finds an abnormality and suspects the wet form of macular degeneration (abnormal blood vessels), a special test called fluorescein angiography will be done. To do the test, dye is injected into a vein in the arm. The dye travels through the body including the eyes. With a special camera (not X-ray), a series of photographs of the retina is taken as the dye passes through it.
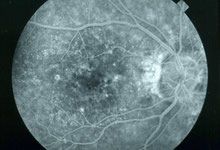
The photographs show what changes have occurred in the retina and where those changes are located. Fluorescein angiography is necessary if the doctor thinks there is a chance that the patient could benefit from laser treatment. The photographs provide a kind of map that the doctor uses during laser treatment. Fluorescein angiography is also usually done a few weeks following laser treatment to be sure that the laser has destroyed the abnormal blood vessels.
There is another photographic test called indocyanine green angiography. This test may give additional information that may be helpful if laser treatment is to be done.

If you would like more information about Fluorescein Angiography, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Macular Degeneration Treatment
Wet Macular Degeneration Treatment
Treatment for wet age related macular degeneration is undergoing major shift from primary laser therapy to pharmacologic therapy with intraocular injection
of drugs that counteract VEGF. VEGF (vascular endothelial growth factor) is a natural chemical in the body necessary for growth of new blood vessels especially for healing. Unfortunately, VEGF appears to be a major factor in the development of wet ARMD. New agents have been developed to counteract VEGF. These agents are injected into the eye at regular intervals, usually about 4 to 6 weeks apart. The results so far have been very exciting.

The first anti-VEGF agent approved was MACUGEN. Macugen is given every 6 weeks. It showed a positive result but only about 6% of patients actually improved in the study group.
Genentech has developed a new drug called Lucentis. Lucentis is very strong anti-VEGF agent. Study results released recently showed 95% of study patients stayed the same or improved with treatment after 2 years. Lucentis has been proven safe and effective in rigorous clinical trials. Lucentis was approved by the FDA and Medicare on June 30, 2006. It is very expensive. One dose costs upwards of $2000. Monthly intraocular injections of Lucentis may be required to obtain the excellent visual results obtained by the studies conducted with Lucentis. Eyelea, developed by Regeneron is a VEGF-trap which effectively prevents the damaging effects of VEGF within the neovascular membrane. It is approximately $1800 per dose, but is not injected as frequently.
Another anti-VEGF agent is currently being used by retinal specialists around the world. Avastin, originally approved for treatment of colorectal caner, has been found by retinal specialists at Bascom Palmer Eye Insitute to be very effective in treating wet ARMD. Avastin has not been officially approved for treatment of ARMD by the FDA. Avastin is relatively inexpensive, and the doctor also will charge for the injection. Avastin is widely used by retinal specialists around the world.
PDT with Visudyne is very expensive, costing about $2000 for the treatment. Macugen costs about $1250 for the injection and the drug.
Laser Treatment of Macular Degeneration
Treatment for macular degeneration with thermal laser or photodynamic therapy (PDT) with Visudyne combined with the injection of a steroid called Kenalog directly into the eye is still used by many retinal specialists for selected cases. This technique of the so called “cold laser” does not cause a retinal scar. Argon or “hot, thermal laser” is still used in selected cases of wet AMD. When the vessels are under the center of the macula, PDT can be used. Some retinal surgeons are using PDT combined with Avastin in an attempt to limit the number of injections required to stabilize wet ARMD.
Up to now, most cases of age related macular degeneration (ARMD) ended up with loss of vision over time with or without therapy. However, with therapy, the final vision plateaus far above what the vision would have been without therapy. With these new anti-VEGF therapies, vision in some cases may actually improve. Clinical trials with Avastin, Lucentis, and Eyelea resulted in 95% of patients staying the same or getting better, while about 40% actually improved with treatment.
Argon Laser
The Argon laser beam is a high energy light that turns to heat when it hits the parts of the retina to be treated. This heat destroys the abnormal blood vessels, causing the wet macular degeneration and stops them from growing, leaking and bleeding. A scar forms as a result of the treatment.
Even when laser treatment is considered successful, and the abnormal blood vessels have been destroyed, additional abnormal blood vessels can appear later and further damage vision. The patient who is treated with laser should continually check the vision in the treated eye and tell the doctor immediately if there are new changes, such as a return of distortion or blurriness; in some cases additional laser treatment may be helpful.
Dry Macular Degeneration Treatment
Although prevention of AMD (age related macular degeneration) is a goal not yet reached by medical research, recent studies (The Age Related Eye Disease Study) have shown that if you have early macular degeneration, taking special vitamins can help reduce the risk of severe vision loss.
If you would like more information about Macular Degeneration Treatment, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Retinal Vein Occlusion
The retina is a thin sheet of nerve tissue in the back of the eye where light rays are focused and transmitted to the brain. Tiny blood vessels supply the retina with oxygen and other nutrients. Arteries deliver the blood, and the retinal veins carry it out. Sometimes one of these arteries hardens or swells and presses on a nearby vein. The vein can then become blocked, or occluded, making it difficult for blood to leave the eye. This is called a retinal vein occlusion (RVO). It is also known as venous stasis retinopathy or hemorrhagic retinopathy. The blocked circulation can lead to swelling, bleeding, growth of abnormal blood vessels, and partial or total vision loss.

Retinal vein occlusions are the second most common cause of blood vessel-related vision loss (the first is diabetic retinopathy). The condition occurs most often in men and women over the age of 50, particularly those in their 60s and 70s. Risk factors include high blood pressure, high cholesterol, diabetes, smoking, glaucoma, and, rarely, blood clotting and inflammatory conditions.
Treatment depends on the severity of the blockage and the location of the blocked vein. If the largest vein leaving the eye is affected, the condition is known as a central retinal vein occlusion, or CRVO; otherwise, it is called a branch retinal vein occlusion, or BRVO. BRVOs often occur with no pain or noticeable loss of vision. It is important to have routine eye exams to detect any developing problems early. You can keep tabs on your vision between appointments by closing one eye at a time.
Retinal vein occlusions are detected during a retinal exam. A fluorescein angiogram
may be performed to confirm the diagnosis and/or aid in treatment planning. Indications that an occlusion is present include bleeding in the eye, macular swelling or ischemia (loss of blood supply), and neovascularization - abnormal growth of new blood vessels. The initial bleeding can prevent the ophthalmologist from seeing any other symptoms for three to six months or longer. The patient is monitored during this time until the blood clears.
There is no cure for retinal vein occlusions. Emphasis is placed on risk management, treatment of symptoms and prevention of further vision loss. It is critical to control high blood pressure, high cholesterol, diabetes and other health conditions that increase the risk of vascular hardening, narrowing and blood clotting.
Branch Retinal Vein Occlusions (BRVO)
Macular swelling may be treated with laser retina surgery, anti-VEGF, or steroids. Surgery may be recommended if scar tissue forms on the retina. Neovascularization typically appears six months to a year after the occlusion. It can cause bleeding, retinal detachment and reduced vision in its advanced stages, so laser photocoagulation treatment is recommended to slow or stop vessel growth. If bleeding continues, a vitrectomy may be performed to remove the blood and abnormal vessels and some of the vitreous gel. Vitrectomy can also relieve tension from a retinal detachment.
Central Retinal Vein Occlusions (CRVO)
While laser treatment has proven effective for prevention of complications caused by CRVO, a significant number of patients may benefit from anti-VEGF
treatment. These include neovascularization and neovascular glaucoma, severe and painful high pressure in the eye that can cause substantial vision loss and blindness. Vision lost to CRVO orneovascular glaucoma cannot berecovered. Other treatments such as surgery and steroids may be of use in selected cases.
If you would like more information about Retinal Vein Occlusion, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Vitreous Surgery
Occasionally, a retinal detachment is so complicated and severe that it cannot be treated with either standard scleral buckling
surgery or pneumatic retinopexy. In such cases, vitreous surgery to reattach the retina may be necessary.
Vitreous surgery is performed in an operating room usually under local anesthesia. The vitreous is removed and, therefore, this procedure is called vitrectomy. The surgeon uses a fiber optic light to illuminate the inside of the eye and other instruments inside the eye, such as forceps, and scissors, to do the surgery. The vitreous is replaced during the operation with either clear fluid that is compatible with the eye, or with gas that completely fills the eye. Over time, the fluid (or gas) is absorbed by the eye and replaced by the eye’s own fluid; the eye does not replace the vitreous itself. The lack of vitreous does not affect the functioning of the eye.
Indications
Vitrectomy is required for retinal reattachment in a variety of conditions. For example, scar tissue may grow on the vitreous or the surface of the retina and pull on the retina and detach it. Occasionally, something in the vitreous, such as blood, prevents the passage of light through the eye to the retina. The most common conditions requiring vitrectomy are vitreous hemorrhage
with retinal detachment, proliferative vitreoretinopathy, giant retinal tears, diabetic retinopathy with vitreous hemorrhage and/or traction retinal detachment, epiretinal membrane (macular pucker), intraocular infection (endophthalmitis), trauma, intraocular foreign body, and macular hole. Today vitrectomy is often used to repair retinal detachment in eyes that have already had cataract surgery.
The Procedure
In a vitrectomy, instruments are passed through the sclera into the vitreous cavity. A variety of instruments can be used to remove the vitreous gel and any scar tissue that may be growing on the surface of the retina. A laser probe can be inserted into the eye so that laser treatment can be done during surgery.
Recent advancements in technology have led to smaller instrumentation for vitrectomy surgery. Standard size for vitrectomy was 20-gauge until recently when much smaller 25-gauge instrumentation became available. No suturing is required in most cases. Healing is quicker, pain is less, and the overall experience of vitrectomy surgery is much more comfortable for the patient.
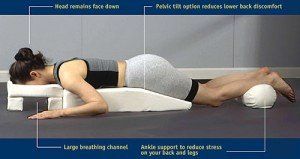
Vitrectomy can be combined with the placement of a scleral buckle. Usually, air, gas, or silicone oil is place in the vitreous cavity. These materials hold the retina in place against the back wall of the eye while the laser scars are forming. After this surgery, it may be important for the patient to maintain a certain position of the head, which is often a face-down (prone) position.

Positioning after vitrectomy surgery with gas bubble present in the eye
Eventually, the gas is absorbed and replaced by fluid produced by the eye. If silicone oil has been used, it frequently must be removed at a later time with another surgical procedure.
Vitreous surgery usually lasts one to two hours but, with very severe and difficult problems, may take longer.
Following surgery, the patient may experience some discomfort and a scratchy sensation in the eye, but significant pain is unusual. If it occurs, the surgeon should be told promptly.
Ultrasonography for Vitreous Hemorrhage and Retinal Detachment
When a retinal tear occurs, retinal blood vessels may also be torn. When this happens, blood enters the vitreous cavity; this is called a vitreous hemorrhage. Because there is a tear in the retina, a retinal detachment
may also occur. The combination of a vitreous hemorrhage and retinal detachment is difficult to treat because the hemorrhage prevents the surgeon from seeing the retina and finding the tears. In such a case, a special technique called ultrasonography is necessary to help make the diagnosis of retinal detachment beneath the hemorrhage.
Ultrasonography is a harmless and painless test. It is like the sonar on a submarine. Sound waves are sent into the eye. They travel through the hemorrhage and bounce off of the retina. The returning sound waves make an image on a monitor and allow the doctor to see whether the retina is attached or detached.
If a patient has a combined vitreous hemorrhage and retinal detachment, a vitrectomy
must be performed to remove the blood so that the surgeon can see the retina. Also, a scleral buckle is placed around the eye. The combination of retinal detachment and vitreous hemorrhage puts the eye at high risk for developing proliferative vitreoretinopathy.
If you would like more information about Vitreous Surgery, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Vitrectomy
Vitrectomy is a microsurgical procedure in which specialized instruments and techniques are used to repair various retinal disorders. The initial step in this procedure is the removal of the "vitreous gel" through a very small micro-incision in the wall of the eye, hence the name "vitrectomy". The vitreous is removed with a miniature cutting device and replaced with a special saline solution similar to the fluid being removed from the eye. An endoilluminator provides the light source used to illuminate the inside of the eye for the surgeon to visualize the internal structures as the surgery is being performed. The surgeon uses a specialized operating microscope and contact lenses, which allow a clear view of the vitreous cavity and retina at various magnifications. The procedure is performed in an operating room under local or (occasionally) general anesthesia. It can, and is often done as an ambulatory procedure. This means that barring complications, a patient is discharged and can leave the hospital or surgical facility within 23 hours. With most of our cases the patients are usually discharged and leave the hospital within 3 to 4 hours of completion of the procedure. Although vitrectomy procedures are sometimes performed through incisions made near the front of the eye, most vitreo-retinal surgeons enter the globe through a part of the eye known as the pars plana. This is why the procedure is often referred to as a pars plana vitrectomy (PPV). Entering the eye through this location avoids damage to the retina and the crystalline lens.

Pars plana vitrectomy (PPV) is used to treat many different retinal disorders including those listed below:
- Proliferative Diabetic Retinopathy
- Vitreous Hemorrhage
- Macular hole
- Macular pucker (epiretinal membrane)
- Certain traction or recurrent retinal detachments
- PVR
- Intraocular infections (endophthalmitis)
- Intraocular foreign body
- Retained lens fragments or dislocated lens implants (following cataract surgery)
- Giant retinal tears
- Certain traumatic eye injuries
The retinal surgeon has at his disposal a variety of specialized techniques and procedures to maximize the effectiveness of vitrectomy surgery, including:
- The use of Intraocular gases, when combined with sterile air, have the necessary properties for remaining in the eye for extended periods of time (up to two months). Eventually, they are replaced by the eye's own natural fluid. Intraocular gases are useful for flattening a detached retina allowing it to remain attached while the healing process takes place. Macular holes are also treated with an intraocular gas injection. An important aspect of gas usage is the requirement for specific head positioning, which varies from case to case, and is discussed with the patient prior to and following surgery. Vision in a gas filled eye is usually rather poor until at least 50% of the gas is absorbed. Possible complications involved in the usage of intraocular gas include an elevation in eye pressure (glaucoma), and the progression of cataracts. It is deemed unsafe to fly in an airplane while intraocular gas remains in the eye as the air bubble will tend to expand.
- Silicone oil is sometimes used instead of gas to keep the retina attached post-operatively. The chemical properties of silicone oil allow it to remain in the eye until removed (often requiring a second surgery at a later date). This technique is advantageous when long term support (referred to as "tamponade") of the retina is required. Unlike intraocular gas injection, patients are able to see through clear silicone oil. The factor of positioning is less critical with silicone oil, and as a result it may be used in patients unable to meet the postoperative positioning requirements (i.e. children). As with gas, silicone oil can promote cataracts, cause glaucoma and cornea damage.
- Endophotocoagulation involves the use of laser
to treat the eye's intraocular structures. This process is often used to treat the retinal tears that may have precipitated a retinal detachment. Endophotocoagulation is also frequently utilized to treat proliferative diabetic retinopathy
as well.
- Scleral Buckling Sugery
where an encircling band is sutured into the sclera, is sometimes combined with a vitrectomy
procedure to add additional support to the reattached retina.
- Lensectomy which involves the removal of the eye's crystalline lens, is usually performed when there is a cataract (a clouding of the lens) preventing the surgeon from adequately visualizing the internal structures. A lensectomy may also prove necessary in gaining access to scar tissue (for its removal) during complicated retinal detachment
or diabetic retinopathy
procedures. The eye's natural lens can be replaced with a clear lens implant at the time of the surgery. Lensectomy is usually performed using high frequency ultrasound (known as phacoemulsification) and is similar to the process involved in routine cataract surgery.
Vitrectomy surgery represents a major medical advance which allows us to treat certain retinal conditions and diseases. It has proved itself successful in preventing vision loss for patients who, prior to the advent of vitrectomy, may have gone blind without this procedure. A vitrectomy usually takes about 1-3 hours or longer depending on the complexity of the case or the combination of other procedures such as scleral buckle or lensectomy. The risks associated with the surgery include infection, bleeding, cataract, glaucoma, and detachment of re-detachment of the retina. These complications can result in severe visual loss, and it is important that you discuss the potential risks and benefits of this procedure with your surgeon before making a decision regarding treatment.
If you would like more information about Vitrectomy, or would like to schedule an appointment, contact us by calling our office directly at (929) 287-3499.
Brooklyn Retinal Vascular Center
185 Montague St.Penthouse Suite
Brooklyn, NY 11201
(929) 287-3499
Website Design
by Hearst Media Services, all rights reserved
HOURS OF OPERATION
Monday - Friday
9:30 am to 4:30 pm
by appointment only
Website Design
by Hearst Media Services, all rights reserved